For healthcare consumers across the USA, ambulatory surgery centers (ASCs) have been providing a much desirable alternative to surgeries taking place in hospitals since their inception in the 1970s.
Ambulatory Surgery Centers (ASCs):
- Provide responsive, non-bureaucratic environments tailored to each individual patient’s needs
- Exercise better control over scheduling, so virtually no procedures are delayed or rescheduled due to the kinds of institutional demands that often occur in hospitals such as unforeseen emergency room demands
- Allow physicians to personally guide innovative strategies for governance, leadership and most importantly, quality improvement
As our nation struggles with how to improve a troubled and costly health care system, the experience of ASCs is a great example of a successful transformation in health care delivery.
Forty years ago, virtually all surgery was performed in hospitals. Waits of weeks or months for an appointment were not uncommon, and patients typically spent several days in the hospital and several weeks out of work in recovery. In many countries, surgery is still performed this way, but not in the US. Physicians have taken the lead in the development of ASCs. The first facility was opened in Phoenix, Arizona, in 1970 by two physicians who saw an opportunity to establish a high-quality, cost-effective alternative to inpatient hospital care for surgical services. Faced with frustrations like scheduling delays, limited operating room availability, slow operating room turnover times, and challenges in obtaining new equipment due to hospital budgets and policies, physicians were looking for a better way―and developed it in ASCs.
Today, physicians continue to provide the impetus for the development of new ASCs. By operating in ASCs instead of hospitals, physicians gain increased control over their surgical practices.1 In the ASC setting, physicians are able to schedule procedures more conveniently, assemble teams of specially trained and highly skilled staff, ensure that the equipment and supplies being used are best suited to their techniques, and design facilities tailored to their specialties and to the specific needs of their patients. Simply stated, physicians are striving for, and have found in ASCs, professional autonomy over their work environment and over the quality of care that has not been available to them in hospitals. These benefits explain why physicians who do not have ownership interest in an ASC (and therefore do not benefit financially from performing procedures in an ASC) choose to work in ASCs in such high numbers.
Given the history of their involvement in making ASCs a reality, it is not surprising that physicians continue to have at least some ownership in virtually all (90%) ASCs. But what is more interesting to note is how many ASCs are jointly owned by local hospitals that now increasingly recognize and embrace the value of the ASC model. According to the most recent data available, hospitals have ownership interest in 23% of all ASCs and 2% are owned entirely by hospitals.2
ASCs also add considerable value to the US economy, with a 2009 total nationwide economic impact of $90 billion, including more than $5.8 billion in tax payments. Additionally, ASCs employ the equivalent of approximately 117,700 full-time workers.
ASCs Provide Care at Significant Cost Savings
Not only are ASCs focused on ensuring that patients have the best surgical experience possible, they also provide cost-effective care that save the government, third party payors and patients money. On average, the Medicare program and its beneficiaries share in more than $2.6 billion in savings each year because the program pays significantly less for procedures performed in ASCs when compared to the rates paid to hospitals for the same procedures. Accordingly, patient co-pays are also significantly lower when care is received in an ASC.
If just half of the eligible surgical procedures moved from hospital outpatient departments to ASCs, Medicare would save an additional $2.5 billion a year or $25 billion over the next 10 years. Likewise, Medicaid and other insurers benefit from lower prices for services performed in the ASC setting.
Currently, Medicare pays ASCs 55% of the amount paid to hospital outpatient departments for performing the same services. For example, Medicare pays hospitals $1,671 for performing an outpatient cataract surgery while paying ASCs only $964 for performing the same surgery.
This huge payment disparity is a fairly recent phenomenon. In 2003, Medicare paid hospitals only 16% more, on average, than it paid ASCs. Today, Medicare pays hospitals 82% more than ASCs for outpatient surgery. There is no health or fiscal policy basis for providing ASCs with drastically lower payments than hospital outpatient departments.
In addition, patients typically pay less coinsurance for procedures performed in the ASC than for comparable procedures in the hospital setting. For example, a Medicare beneficiary could pay as much as $496 in coinsurance for a cataract extraction procedure performed in a hospital outpatient department, whereas that same beneficiary’s copayment in the ASC would be only $195.
Without the emergence of ASCs as an option for care, health care expenditures would have been tens of billions of dollars higher over the past four decades. Private insurance companies tend to save similarly, which means employers also incur lower health care costs when employees utilize ASC services. For this reason, both employers and insurers have recently been exploring ways to incentivize the movement of patients and procedures to the ASC setting.
The long-term growth in the number of patients treated in ASCs, and resulting cost savings, is threatened by the widening disparity in reimbursement that ASCs and hospitals receive for the same procedures. In fact, the growing payment differential is creating a market dynamic whereby ASCs are being purchased by hospitals and converted into hospital outpatient departments. Even if an ASC is not physically located next to a hospital, once it is part of a hospital, it can terminate its ASC license and become a unit of the hospital, entitling the hospital to bill for Medicare services provided in the former ASC at the 81% higher hospital outpatient rates.
Anesthesia management in ASCs
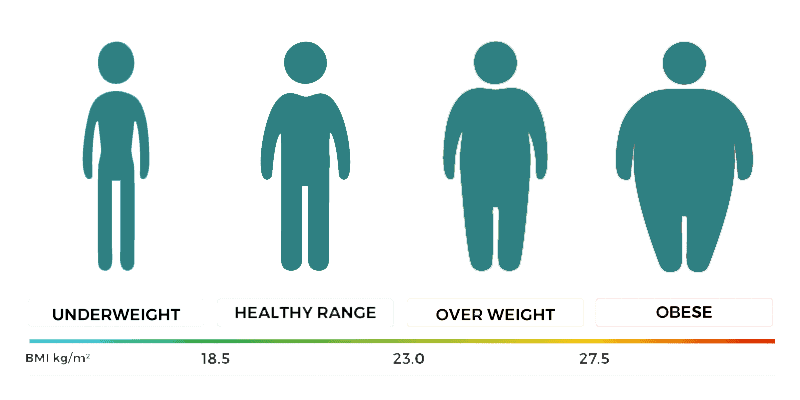
With today’s better understanding of the pharmacology of anesthetic drugs and techniques, anesthesia management plans can be modified to reduce complications in patients with obesity. Minimizing or completely avoiding sedatives and opioids increases the safety of anesthesia for patients with morbid obesity. Inadequate or over-treatment of postoperative pain in the patient with morbid obesity will negatively impact postoperative recovery.
Opioid-only analgesic regimens are usually avoided because of their unacceptable respiratory-depressant side-effects in patients with morbid obesity. Balanced “multi-modal” analgesia combining regional or local analgesia when possible with nonopioid analgesic drugs, and giving opioids only in small amounts as rescue agents, is the best approach for treating postoperative pain. Intravenous (IV) infusions of either remifentanil or dexmedetomidine reduce the intraoperative use of opioids and decrease time spent in the postanesthesia care unit (PACU), in turn leading to earlier home discharge with fewer complications.
Likewise, the occurrence of postoperative nausea (PN) with or without vomiting can prolong PACU stay or even lead to admission to a hospital. Generous amounts of IV fluids and multimodal prophylactic drug therapy with dexamethasone plus other agents will reduce the incidence and severity of PN, but cannot totally eliminate its occurrence.
Selim Surgery Center uses an experienced anesthesia group. This group is formed of trained and experienced anestheiologists with the help of their experienced CRNAs (certified registered burse of anethesia). It is the same group that provides anesthesia for Dr Selim at other hospitals.