They are defined as:
- abnormal or excessive fat accumulation that may impair health;
- have important consequences for morbidity, disability and quality of life;
- entail higher risk of developing type 2 diabetes, cardiovascular diseases, several common forms of cancer, osteoarthritis and other health problems; and
- are serious public health challenges according to the WHO.
Obesity is common, serious, and costly
- According to the CDC (Center of Disease Control) and WHO (World Health Organization), in 2015~2016, the prevalence of obesity was 39.8% and affected about 93.3 million of US adults.
- Obesity-related conditions include heart disease, stroke, type 2 diabetes and certain types of cancer that are some of the leading causes of preventable, premature death.
- The estimated annual medical cost of obesity in the United States was $147 billion in 2008 US dollars.
- The medical cost for people who have obesity was $1,429 higher than those of normal weight.
Obesity affects some groups more than others
- Hispanics (47.0%) and non-Hispanic blacks (46.8%) had the highest age-adjusted prevalence of obesity, followed by non-Hispanic whites (37.9%) and non-Hispanic Asians (12.7%).
- The prevalence of obesity was 35.7% among young adults aged 20 to 39 years, 42.8% among middle-aged adults aged 40 to 59 years, and 41.0% among older adults aged 60 and older.
Obesity key acts
- Worldwide obesity has nearly doubled since 1980.
- In 2008, more than 1.4 billion adults, 20 and older, were overweight. Of these over 200 million men and nearly 300 million women were obese.
- 35% of adults aged 20 and over were overweight in 2008, and 11% were obese.
- 65% of the world’s population live in countries where overweight and obesity kills more people than underweight.
- Overweight and obesity are the fifth leading risk for global deaths. At least 2.8 million adults die each year as a result of being overweight or obese.
- 44% of the diabetes burden, 23% of the ischaemic heart disease burden and between 7% and 41% of certain cancer burdens are attributable to overweight and obesity.
- More than 40 million children under the age of five were overweight in 2011.
- Obesity is preventable.
Obesity and socioeconomic status
The association between obesity and income or educational level is complex and differs by sex and race/ethnicity.
- Overall, men and women with college degrees had lower obesity prevalence compared with those with less education.
- By race/ethnicity, the same obesity and education pattern was seen among non-Hispanic white, non-Hispanic black, and Hispanic women, and also among non-Hispanic white men, although the differences were not all statistically significant. Although the difference was not statistically significant among non-Hispanic black men, obesity prevalence increased with educational attainment. Among non-Hispanic Asian women and men and Hispanic men there were no differences in obesity prevalence by education level.
- Among men, obesity prevalence was lower in the lowest and highest income groups compared with the middle income group. This pattern was seen among non-Hispanic white and Hispanic men. Obesity prevalence was higher in the highest income group than in the lowest income group among non-Hispanic black men.
- Among women, obesity prevalence was lower in the highest income group than in the middle and lowest income groups. This pattern was observed among non-Hispanic white, non-Hispanic Asian, and Hispanic women. Among non-Hispanic black women, there was no difference in obesity prevalence by income.
The studies showed that being overweight or obese is associated with a higher risk of dying prematurely. The risk increases with additional pounds or additional waist ratio, according to a large international collaborative study led by researchers at the Harvard T.H. Chan School of Public Health and the University of Cambridge, UK. The findings contradict recent reports that suggest a survival advantage to being overweight—the so-called “obesity paradox.” The study was published online on July 13, 2016 in The Lancet.
The serious effects of obesity on chronic disease have been well documented. In order to provide more definitive evidence for the association of excess body weight with premature mortality, researchers joined forces in 2013 to establish the Global BMI Mortality Collaboration, which involves over 500 investigators from over 300 global institutions.
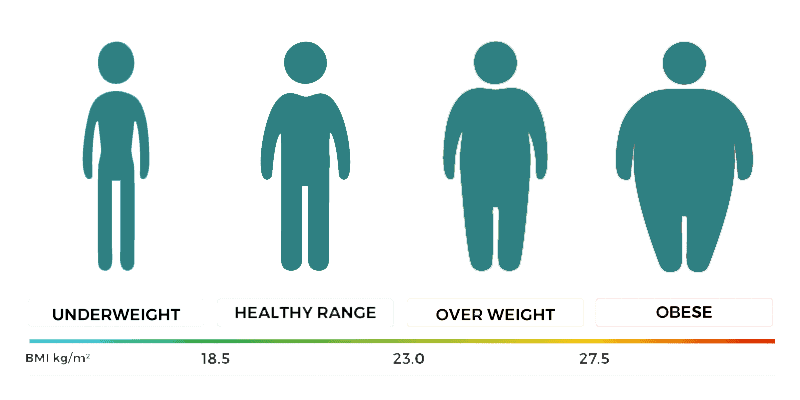
Harvard University has published a new study where consortium researchers looked at data from more than 10.6 million participants from 239 large studies, conducted between 1970 and 2015, in 32 countries. A combined 1.6 million deaths were recorded across these studies, in which participants were followed for an average of 14 years. For the primary analyses, to address potential biases caused by smoking and preexisting diseases, the researchers excluded participants who were current or former smokers, those who had chronic diseases at the beginning of the study, and any who died in the first five years of follow-up, so that the group they analyzed included 4 million adults. They looked at participants’ body mass index (BMI)—an indicator of body fat calculated by dividing a person’s weight in kilograms by their height in meters squared (kg/m2).
According to Harvard, the results showed that participants with BMI of 22.5-<25 kg/m2 (considered a healthy weight range) had the lowest mortality risk during the time they were followed. The risk of mortality increased significantly throughout the overweight range: a BMI of 25-<27.5 kg/m2 was associated with a 7% higher risk of mortality; a BMI of 27.5-<30 kg/m2 was associated with a 20% higher risk; a BMI of 30.0-<35.0 kg/m2 was associated with a 45% higher risk; a BMI of 35.0-<40.0 kg/m2 was associated with a 94% higher risk; and a BMI of 40.0-<60.0 kg/m2 was associated with a nearly three-fold risk. Every 5 units higher BMI above 25 kg/m2 was associated with about 31% higher risk of premature death. Participants who were underweight also had a higher mortality risk.
Looking at specific causes of death, the study found that, for each 5-unit increase in BMI above 25 kg/m2, the corresponding increases in risk were 49% for cardiovascular mortality, 38% for respiratory disease mortality, and 19% for cancer mortality. Researchers also found that the hazards of excess body weight were greater in younger than in older people and in men than in women.
Obesity Related Health Diseases
As mentioned above, obesity is a serious condition that can compromise your health, happiness, and longevity. Obesity forces the organs—especially the heart and lungs—to work harder, and it places excessive stress on the joints.
Obesity can cause, worsen, or increase your risk of several health conditions, including:
- Sleep apnea
- Diabetes mellitus
- High blood pressure (hypertension)
- High cholesterol (hyperlipidemia and hypercholesterolemia)
- Infertility and sexual dysfunction
- Fatty liver (excess fat in the liver that can lead to inflammation and liver damage)
- Heart attacks
- Strokes
- Joint pain and osteoarthritis
- Polycystic ovarian syndrome (a hormone imbalance that can disrupt menstruation and ovulation)
- Cancer (obesity increases the risk of some cancers)
- Depression
The Weight Loss Surgery Program at Selim Surgery Center is designed for patients who have exhausted traditional methods of achieving lasting weight loss. We offer several weight loss procedures that are well established as safe and effective.